
How Seniors Can Sleep Better
Sleep is one of the most important things we do for our health.
When a senior — or anyone — is sleeping poorly, it could be a symptom of a larger problem, like anxiety, or an undiagnosed illness. But sleeping better can also help cure these problems.
So for any seniors struggling with their health, a good first question is: “Are you sleeping well?”
More often than not, the answer will be: No. Half of seniors report some sort of sleep problem. Some of the most common sleep problems among older folks are:
- Taking longer to fall asleep
- Not sleeping as much
- Waking up more often during sleep
- Not feeling refreshed after sleep
- Feeling drowsy during the day
- Napping more often and longer
When we’re young, stress is the most common cause of restless sleep or fragmented sleep. As we age, sleep problems are more likely to be caused by a physical issue. Studies show that 81 percent of arthritis patients, 85 percent of those suffering from chronic pain, and 33 percent of diabetes patients report difficulty staying asleep.
Changing Sleep Patterns Are Normal
As we get older, our sleep changes. One study of men aged 16 to 83 found that total sleep time decreased on average by 27 minutes per decade. Older people are more likely to wake during the middle of the night. They also spend less time in deep sleep.
What’s going on here? It’s a natural part of aging, just like our eyesight or 100-meter dash time getting worse. The part of the brain that regulates our body clock deteriorates as we get older. And decreasing levels of melatonin, a chemical associated with helping people get to sleep, doesn’t help either.

But here’s the thing. These factors all affect seniors broadly — they don’t tell you exactly why you, your patient, or your loved one isn’t getting a good night’s sleep.
Is it because their body chemistry is changing? Or because they aren’t exercising as much? Are they a workaholic, no less ambitious and stressed out than any career-obsessed thirty-something? Any of these are possible causes. Everyone’s different.
If you’re a senior, or you’re taking care of one, it’s not as important to understand why someone isn’t sleeping well than it is to get back to those regularly scheduled trips to dreamland. Yes, slightly more than half of seniors report sleep problems, but that means that there are plenty of seniors sleeping just fine.
This guide focuses on what seniors, and their caretakers, can do to increase their amount of sleep and promote high quality sleeping.
Why Sleep Quality Is More Important Than Hours Slept
Imagine you asked someone about their diet and they said: “I eat every day.” Great news, but not very illuminating. Eating every day could mean two eggs for breakfast, a salad for lunch, and a small piece of fish with brown rice for dinner. It could also mean a steady intake of TV dinners and cupcakes.
You may be getting enough sleep according to your health care provider, however, you aren’t getting good sleep. Many Americans are unaware of their sleep problems: a national poll done by NSF showed that 80% of respondents had undiagnosed sleep apnea. Why is this the case? Sleep quality is trickier to measure — but it’s just as important. To understand how someone is sleeping, you first have to understand the sleep cycle.
Successful sleep follows a pattern, which experts divide into four stages. Scientists discovered this pattern about 100 years ago, using machines that detect brain waves as we sleep.
- Stage 1 (Drifting Off)
- Stage 2 (Light Sleep)
- Stage 3 (Deep Sleep)
- Stage 4 (REM Sleep)
Let’s talk about each stage and what it means:
Drifting Off (Stage 1)
You might not even consider this sleep. It’s at that edge between sleep and wakefulness. You’re somewhat aware of your surroundings, but wouldn’t want to operate any heavy machinery. This type of sleep occurs at the beginning of the night, and may not recur. Most people spend somewhere between 10-25 minutes in stage 1.
Light Sleep (Stage 2)
Your body is still on alert — you’re more likely to wake up during Stage 2 sleep than in Stages 3 or 4. Still, you’re actually getting the benefits of sleep during this stage. Tests have shown that your mind is consolidating memories during this phase. If you take power naps, this is likely the sleep stage you’re getting to. An average, eight-hour sleeper, would spend about four hours in Stage 2 sleep.
Deep Sleep (Stage 3)
This is the closest we humans get to hibernation. Heart rate and breathing decreases, and the brain is dormant. During deep sleep, our body is resting and recuperating. Around two hours of an average night of sleep is spent in Stage 3.
REM Sleep (Stage 4)
Rapid Eye Movement (REM) sleep intrigues and mystifies sleep researchers. Not everyone experiences REM sleep, and even those who do can go long stretches without it. REM sleep is associated with dreaming — when you wake from a vivid dream, you were likely in the middle of REM sleep.
Most people will progress through all four stages at the start of sleep. This takes about an hour. After that, the body cycles back through stages 2, 3, and 4, with the period of REM sleep getting longer and longer throughout the night. Often, people will wake directly during REM sleep.
The amount of REM sleep decreases as we age — from about eight hours at birth to two hours at age 20 to only about 45 minutes at age 70. But science can’t really tell us why, or what it means. And, again, these are all averages. Seniors shouldn’t give up on having high-quality sleep just because they are older.
Seniors with high-quality sleep should report:
- A limited period of restlessness before falling asleep.
- Minimal interruptions during the night.
- Feeling refreshed — not groggy — when they wake up.
If one of these three boxes goes unchecked, that means there’s room for improvement. Which is not a bad thing! Don’t think of poor sleep as a problem, think of it as an opportunity. Better sleep could fix a lot of other problems that a senior is writing off as the costs of aging.
Sleep Problems In Older People
Nearly half of people over the age of 60 say they have trouble getting to sleep. That’s the bad news. The good news is that, unlike with younger people, it’s usually easier to isolate the cause of insomnia in the elderly. More than 90 percent of the time, an older person’s insomnia is due to one of these:
- Circadian rhythm changes
- Specific sleep disturbances than can be treated
- Physical illness
- Mental illness
- Medications
- Dementia
- Poor sleep habits
Circadian Rhythm Changes
Older people tend to feel sleepy earlier in the day than they used to, and wake up earlier. It’s a natural part of aging. That’s why the National Sleep Foundation sleep recommendations for people 65 and older maxes out at eight hours — for folks aged 25-64, nine hours may be necessary.
Older people should listen to their bodies. Typically, those who try to stay awake later than their body wants to will wake up early anyway. Eventually, sleep deprivation will set in.
For older people who live in institutions, it can be difficult to get enough daylight — studies have shown that people in nursing homes see as little as 10 minutes of bright light per day. The low, artificial light confuses the body, which doesn’t know what the real time is, and contributes to frequent napping.
Bright-light therapy has been shown to help these people maintain a more standard sleep schedule. Any older person who spends too much time inside may be prone to a damaging lack of daylight.
Sleep Apnea and Snoring
The medical term is “Sleep-Related Breathing Disorders,” but we know it as sleep apnea or snoring. People of any age — even children — can experience severe snoring or difficulty breathing that interrupts the sleep cycle. In its extreme form, sleep-disordered breathing is also known as sleep apnea. People who experience snoring or sleep apnea may not even realize it’s happening — they just feel very groggy when they wake up.
Obstructive sleep apnea is the most common form of sleep apnea. This can occur when your throat muscles block your airway while sleeping, causing snoring and difficulty breathing. Some signs of obstructive sleep apnea include: snoring, periods of stopped breathing during sleep, gasping or choking, and awakening with a dry or sore throat.
A senior who thinks they may be suffering from this health condition should consult a doctor immediately. This is a potentially life-threatening problem. Treatment can include anything from lifestyle changes (like losing weight) to equipment that helps the person breathe during the night, and promote healthy sleep patterns.
Restless Leg Syndrome and Other Limb Movements
Hospitals estimate that 5 to 10 percent of people experience some form of restless legs syndrome. It’s an uncomfortable sensation that causes an uncontrollable urge to move your legs, especially while you are resting. Although the movement temporarily relieves the uncomfort, it makes it more difficult to go to sleep. The phenomenon is more common among older adults, and often worsens as people age.
Another limb movement issue, Periodic Limb Movement Disorder, is similar to snoring because it occurs during sleep and can go unnoticed.
Seniors should talk to their doctor if they experience either of these limb movement issues, even if it only happens a few times a month. Anything that affects the ability to sleep is a problem worth addressing.
REM Sleep Behavior Disorder (RSBD)
REM sleep is often associated with vivid dreaming. In this state, the body is immobile. People with REM Sleep Behavior disorder, however, begin to act out their vivid dreams — flailing and shouting in reaction to the events in the dream.
Men over the age of 50 are more likely to experience RSBD. It can be embarrassing for people to talk about. But, because it interrupts REM sleep, it affects sleep quality overall. It can also affect the sleep quality of the senior’s partner. In advanced cases, the person can injure themselves or their partner. RSBD can be a sign of a more critical neurological disorder. It can also be a side effect of medication, especially antidepressants.
Medical (Physical) Illness
It’s common sense that you won’t sleep as well when you’re sick or in pain. Surveys back this up. More than 8 in 10 older adults with knee painsaid they had trouble staying asleep. People with diabetes arefour times more likely to report sleep problems.
This creates a vicious cycle, because sleep is healing. A serious medical condition is unlikely to improve if the person isn’t sleeping well. As seniors recover from medical issues, they and their caregivers should be even more attentive to sleep issues than normal.
Mental (Psychiatric) Illness
At all ages, mental illness and insomnia are closely linked. Insomnia can be a result of suffering from depression. Lack of sleep can also be an indicator that someone is at risk of developing a psychiatric disorder. The clear message: Our minds need sleep. Improved sleep quality can be part of the treatment for an existing mental illness, and can help prevent a future one.
Dementia and Sleep Disruption
Most dementia patients experience some form of sleep disruption, and the disruption tends to get worse as the disease progresses. The specific form of sleep disruption will depend on the patient, and likely depends on how the dementia is affecting their mind.
Some of the sleep disorders suffered by dementia patients get so bad, the patient needs to be institutionalized. REM Sleep Behavior Disorder, often associated with Lewy Body Dementia, can result in patients causing injury to themselves or their sleeping partners. Nighttime wandering or “sundowning” — increased agitation during the early afternoon or evening — can also be too much for home caregivers to deal with.
Typically, doctors will try to identify the specific sleep problem and treat it just as they would with a non-dementia patient. Dementia patients are no different than anyone else — they need sleep to heal.
High Blood Pressure
New research has shown that those who have trouble falling asleep and get less sleep at night are also more at risk for high blood pressure. Those suffering from chronic insomnia and are highly alert during the day may have an increased secretion of stress hormones, which can lead to hypertension. Over a long period of time, it can even lead to an overall decline in physical health and heart disease.
Those who already have high blood pressure should watch how many hours of sleep they are getting. Doctors recommend getting at least 7 to 8 hours of sleep at night to control the body’s hormones, and keep blood pressure at a steady level.
Medications
Many of the most common medications prescribed to elderly folks are known to interfere with sleep. Seniors and their caregivers should monitor sleep quality closely after starting a new medication. If a medication is interfering with sleep, most doctors will find an alternative. If the medication is critical, a pre-sleep sedative may be prescribed. The body can’t live without sleep, and any treatment regimen must take that into account.
What To Change To Sleep Better
The three main factors leading to less sleep are:
- Routine — When you sleep, and what you do immediately before that.
- The Sleep Environment — Where you’re sleeping, and what you’re sleeping on.
- Diet & Exercise — What you eat, and how often you move.
We’ll take a look at each factor — what it means, and how to set it for maximum effectiveness.
Routine
Sleep researchers believe that the more consistent your evening routine is, the better your sleep will be. You surely have some form of sleep routine already — brushing your teeth, putting on your pajamas, stalking the grandkids on Facebook.
If you’re having trouble getting to sleep, or staying asleep, try making this routine more regimented. Turn it into a schedule.
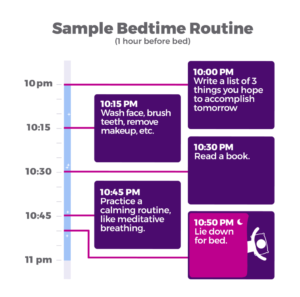
These are just guidelines. There is no “best time to sleep” for everyone, just one that works for you. Your sleep routine should include whatever you feel will put you in a relaxed frame of mind — and on the express train to Dreamtown.
One suggestion that isn’t in everyone’s toolkit — some sort of mindfulness practice. If you do a nightly prayer, that’s a form of mindfulness. If that’s not your thing, mindfulness could take the form of meditation, listening to calming music, or writing letters of advice to your less successful grandkids. Dr. Andrew Weil, the Harvard-trained doctor and author, promotes a breathing technique, the 4-7-8. Here he shows you how to do it:
https://www.youtube.com/watch?v=gz4G31LGyog
The Sleep Environment
Most of us only think about our sleep environment when it gets disrupted. An extremely hot night. A partner with a persistent cough. A neighbor learning the trombone. But what about the basics: Is your room a place of peace? Is your bed comfortable? If you aren’t sleeping well, it might be time to experiment.
Temperature
Our bodies are used to sleeping at night, as the temperature cools down. If your bedroom is too hot, your body may simply be confused. One simple step to getting better sleep? Try setting the thermostat a tick or two lower. If you can’t control the temperature of your bedroom, fans can make you feel cooler. It’s okay to trick your body for its own good.
Light
The whole sleeping at night thing also means our bodies expect darkness. Fewer and fewer of us have it. Modern bedrooms often have larger windows. And, because the heavy curtains of the English country house are so expensive, we tend to cover them with thin paper or metal blinds. Cities and suburbs are brighter at night than they used to be. To sum up, everyone before you in the family tree probably slept in a darker bedroom than you do.
We’re not suggesting you go sleep in a cave, but you might benefit from a room that’s lit like one. Blackout curtains are inexpensive and easy to install. Figure out how to dim any electronics that toss light at night. Or, invest in an eye mask.
Important: If your bedroom is too dark, you might be risking a fall if you need to get up in the middle of the night. Keep light within arm’s reach of your bed at all times, whether that’s a lamp, a flashlight, or your iPhone.
With that being said, keep your usage of electronic devices to a minimum before bed. Devices such as smartphones and televisions give off blue light, which blocks our body’s release of melatonin and can offset our circadian rhythm. Try using blue-light-blocking glasses at night, or turning off electronics 2 to 3 hours before bedtime.
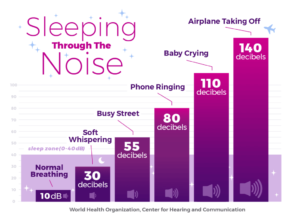
Noise
Persistent noise during sleep not only prevents you from sleeping, but it might lead to something even more dangerous. Trying to sleep when the noise level is 55 decibels or above, or about what a busy street sounds like, can cause higher blood pressure and heart attacks.
Unexpected sounds from passing cars, night-owl neighbors, or clumsy partners can drop you straight out of your dream cloud. If outside noises are disturbing your sleep, heavy curtains can help block them out. A white noise machine or “soothing sounds” recordings may help relax you. Finally, the brute force method — ear plugs.
The Bed
Humans have prepared a special place for sleeping for a long time — archaeologists have found 77,000-year-old mattresses in a cave in South Africa. These cave dwellers slept on thin mats of woven grass. Your bed is probably a little more comfortable, but that doesn’t mean it’s as comfortable as it should be. If you are having trouble sleeping, and especially if you experience pain during or after sleep, it’s worth thinking about switching up your sleep tech.
Be picky. Reputable mattress manufacturers and sellers know how important your sleep is, and offer generous return policies. If you think your mattress is keeping you from getting your best night’s sleep, try a new one. Or a new pillow and sheet set. If you still don’t sleep well you should be able to return them and try something else.
Mattress
Does your mattress feel too hot? Do you feel pressure points on certain parts of your body while you’re trying to sleep? If you sleep with a partner, do you feel them moving around? Any of these problems could indicate that you need to upgrade your mattress.
Sheets
Sheets should be smooth and provide a comfortable temperature while you sleep. If you feel cotton threads on your sheets, they are fraying — it may be time to buy new ones.
People who like to feel warm when they sleep often invest in flannel sheets. Among cotton sheets, percale are said to feel cooler, while satin are said to feel warmer. Some people prefer linen sheets, which are expensive but some people find them more breathable. Bamboo sheets are a relatively new innovation. It’s all personal preference here, but if you’re sleeping poorly, it’s worth considering a switch.
Blanket
Some folks report higher quality sleep using a weighted blanket. The pressure could serve as a form of touch therapy, bringing a feeling of peace and safety. On the other hand, a blanket may be the cause of sleep problems if it is keeping you too warm.
Pillow
If you experience neck pain or discomfort during or after sleep, your pillow is likely to blame. A subpar pillow won’t give your neck proper support during the night, and can lose its shape over time.
The material of your pillow could also be trapping heat. Heating pads have a place in the bed, but it’s not on your face.
Diet & Exercise
Sleep is a critical part of our overall health — along with diet and exercise. Not surprisingly, if you’re not giving your body the nutrients it needs, and not providing the movement it expects, your sleep will suffer.
What we eat — and when we eat — can help or hurt our sleep quality. And, just like with physical maladies, the process works in reverse. Many studies have shown that people who sleep more tend to eat better and are less likely to be obese.
Spicy/Rich/Fatty Foods
Let’s start with the obvious — heartburn or a stomach ache is going to make it harder to fall asleep, just as a headache or knee pain will.
But even if you pass out right after eating your nightly herb-buttered tomahawk steak, you could improve your sleep quality by choosing the fish fillet and steamed broccoli instead. ”Intervention diets” that reduce fat and carbohydrate intake have been shown to help reduce Stage 1 sleep, and increase REM sleep.
Caffeine, Alcohol, Sugary Drinks, Tobacco
Substances meant to keep us alert or in a festive spirit can also make it hard for us to sleep.
Caffeine and sugar are both stimulants, so it stands to reason that they can prevent us from falling asleep. Alcohol can help you fall asleep, but it won’t be a good sleep. Studies have shown that when alcohol is in your system, you get less deep sleep.
The good news is that our bodies process these substances fairly quickly. So, as long as you aren’t ingesting them in the few hours before you go to sleep, they shouldn’t cause problems. Anyone having trouble sleeping should consider avoiding these substances in the hours before bedtime.
Eating Late
Eating a large meal before bed has been linked with insomnia. If you’re having trouble sleeping, consider eating earlier, or eating more at breakfast or lunch. Snacks are okay, though — here are the ten best foods to eat before bed.
Liquids
The more you drink before bed — whether it’s milk, water, or panda poop tea — the more likely it is that your bladder will scream out for assistance mid-doze. Limiting your liquid intake could improve your sleep quality.
Exercise
Bodies that remain in motion are more likely to successfully stay stationery during sleep time. This probably conflicts with one of Newton’s Laws, but it is a scientific fact that our bodies were designed to move — no matter what our age is. And, just as with our diet, an increasing “body” of scientific work shows that the relationship works both ways. People who don’t sleep well tend not to move as much.
Any older adult who isn’t sleeping well may benefit from moving their bodies more. This movement doesn’t have to take the form of joining a gym.
A worldwide study of the places with the most centenarians revealed that their movement didn’t take the form of traditional exercise. Instead, they stay active with natural movements like sitting on the floor and standing up, or doing chores without the use of appliances.
In a 2010 study, adults 55 and older who suffered from insomnia and lived sedentary lifestyles were separated into two groups. One group started an exercise program. The other group remained sedentary. The results showedsignificant sleep quality improvements for participants who exercised.

What To Do About Persistent Sleep Problems
Anyone, of any age, who has trouble sleeping should talk to their doctor. Your primary care doctor has the best picture of your overall health, and will have suggestions — many of which may match some of the medicines and recommendations above.
If sleep quality continues to be a problem, your doctor will likely recommend that you undergo a sleep study. During a sleep study — an overnight exam held at a specialized facility — experts monitor your hours of sleep and try to diagnose your sleep issues.
The U.S. has more than 2,500 accredited sleep centers. This finder from the American Academy of Sleep Medicine can help you identify the nearest one.
Some of the top national sleep centers include the Cleveland Clinic Sleep Disorders Center and the Mayo Clinic Center for Sleep Medicine. Both of these facilities employ doctors from different medical specialties, all of whom also specialize in sleep. Challenging sleep problems probably involve more than one part of your body.
Doctors and scientists are only just beginning to understand how and why we sleep. But one thing they can say for sure: Everyone’s body, no matter how old it is, wants to sleep.
When we’re improving sleep, we’re not forcing our body to do something it doesn’t want to do. We’re just giving it a little bit of help.
“This article originally appeared on Purple.com“
Northfield Retirement Communities offers trustworthy and professional rehabilitation, Independent Living, Assisted Living, Skilled Nursing and other specialty Aging Services.
Call 308.632.4342 for more information.

